Injuries
Runner injuries are always an important point of discussion between athletes and Patellofemoral Pain Syndrome is the more common injury. Every athlete will have been through an injury period and it is always a tough mental time. Looking at the statistics, the majority of the injuries are between the knee and the foot. The top five injuries with runners are:
1 – Patellofemoral Pain Syndrome (PFPS) – Runner’s knee
2 – Achilles Tendon injury
3 – Plantar Fasciitis
4 – Shin splints
5 – IT band
Another common injury is the hamstring injury.
The main causes of injuries are the increase in the training load too quickly and a previous injury. To avoid injuries, ensure you increase the load very progressively and if you get injured, get the physio to improve the situation and work on your rehabilitation up to the end of the treatment.
To lower risks of injuries, apart from the running, you should work on the drills before the speed sessions and add the following sessions: plyometric, hills reps, Strength and Conditioning.
Disclaimer concerning this article: I give general advice based on my knowledge gained during my sport massage therapy course and readings. This article is not replacing the judgement of a doctor or a physiotherapist. Ensure you visit your local doctor or therapist for a detail analysis of your injury.
What to do when you get an injury:
First, the most important is to stop your run / session. Do not run on an injury. Take a taxi, ask a drive back home or walk back. However, do not continue your run.
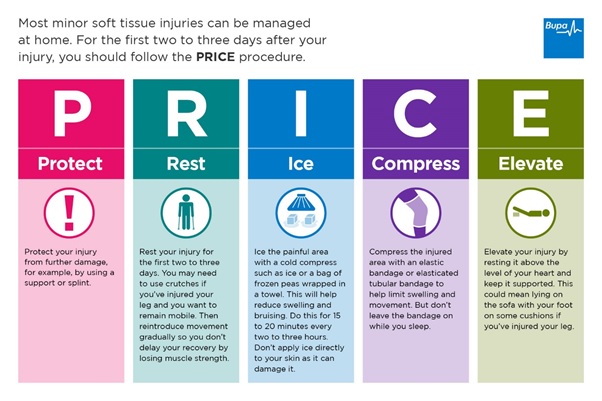
Secondly, when you are at home, you need to follow the PRICE treatment for the next 48 hours to 72 hours until the inflammation is gone:
– Protect the area.
– Rest: avoid walking too much, do not do any sport. If the pain is very acute, use crutches.
– Ice: This is a bony area, then you should ice only for 5 minutes at a time. Ice three to five times per day. Use a cloth to avoid the ice to be in direct contact with the skin. If you have access to the sea, a cold river, you can use the natural water to cool down your full legs. Using ice cubes in a bathtub is an alternative.
– Compress: If there is inflammation of the knee, compress the area.
– Elevate: Ensure the knee is slightly bent. An advice is to put a cushion under the mattress and not directly under to feet.
Third, get an appointment with your physio. The physio will be able to start the treatment after the inflammation.
Fourth, if the physio cannot fully treat and the injury is very serious you need to go to your doctor or specialist. If the injury is serious, go straight to the doctor or to the emergency room of your local hospital.
Reminder
The physio will be able to improve the injury during your visit, but remember that the main improvements are going to come from you. Ensure you do all the exercises given by the physio.
Do not overdo because it can be counter-productive and bring further inflammation, but ensure you do not wait until next appointment to get the physio to improve the situation.
Patellofemoral Pain Syndrome PFPS:
The Patellofemoral Pain Syndrome is the most common injury with athletes. It is even called the “Runner’s Knee”. Another name for this injury is the “Chondromalacia Patella”. The pain is generally at the front of the knee, between the kneecap and the femur. The pain can increase if you stay seating long periods, during use or by climbing or descending the stairs. Female runners are more impacted by this injury.
With the help of Leonardo Da Vinci drawings let’s see the bones and muscles involved:
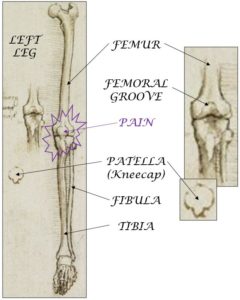
What is happening exactly: The kneecap (patella) is grinding on the femur head. Both the inside of the patella and the femur head are covered with cartilage to avoid the bones to get in direct contact. The patella movement is not aligned and may produce irritation and inflammation.
Symptoms and cause:
The pain is increasing gradually and due to overuse. You can feel pain around the kneecap or just behind it. The pain can be felt by loading the knee (stairs, squats, kneeling, cycling or running). The knee may be doing a “clicking” noise when you bend/extend it.
There are different potential cause for this injury. The main should be the increase in the level of activity (higher load or higher volume). A badly worn pair of shoes or new shoes with a different drop or support may be affecting the knee.
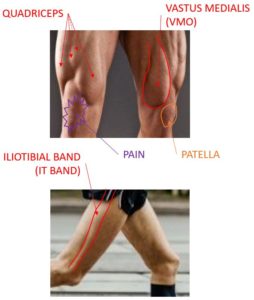
The second cause is the misalignment of the patella in the femoral groove during the knee movement. Muscles above the knee can influence the patella movement:
– The quadriceps muscle imbalance. In most of the cases, the Vastus Medialis (VMO) is weak and the patella is pulled buy the other quads muscle laterally.
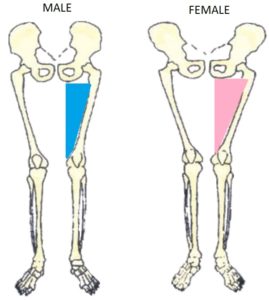
– The hips are weak, and the Q angle of the femur is very high (mainly legs in X shapes). Women have hips with different shapes to allow birth. The hips shape will naturally increase the Q angle and put extra pressure on the knee.
– The last muscle that can influence the patella alignment is the iliotibial band (the IT band). If the iliotibial band is too tight, it will pull the kneecap laterally.
Diagnosis:
The physio will start look at how you walk / run to look at your Q angle, the position of the foot and the hips. Then there are special tests that need to be done:
– The Clarke’s test makes the patella slide in the femoral groove :
– The VMO strength test, will check how strong is your Vastus Medialis muscle:
– The Ober’s test, will check the tightness in the Iliotibial band (IT band):
– Another test will be to load the knee by climbing / descending stairs or squatting and ask the runner to describe the pain.
– The Noble test will check if you have as well an issue on the Iliotibial band:
The doctor may ask for a Magnetic Resonance Imaging, but it will not give more information, because the knee is not loaded. The doctor may ask for an X-ray in order to ensure there is no bone issue in the area.
It is important the diagnosis is ruling our other potential issues in the area (tendinitis, bursitis, Osgood-Schlatter disease…)
Treatment:
It is at this point that the physio will be able to start the treatment in a very specific way. Depending of the root cause defined, the best way to improve is to work on the strength of the weak muscles: Vastus Medialis (VMO), hip flexor and / or gluteus. As usual, the exercises need to be gradual and using different ways to contract the muscles (concentric, eccentric and isometric).
Other treatments may be given by doctors like medication, or by the physio with braces and taping.
If the cause is coming by an over pronation, another improvement can be done mechanically by using insoles. I prefer personally the strengthening, but an insole may be a faster way to compensate the mechanical problem and solve the issue quickly.
To lower the risk of the Patellofemoral Pain Syndrome to happen, work on your strength and add the following to your training:
– 10 to 15 minutes of drills before each speed training session
– One session of plyometric per week
– hills repetitions (at the end of your easy days, 5 to 10 hills repetitions)
– Strength and conditioning (2 sessions per week)
